T wave = electrical recovery
and relaxation of ventricles. A heart attack (myocardial infarction or
MI) can be recognized by an elevation in the S-T segment of the
ECG. Thus, one type of MI is an S-T elevation MI or STEMI.
addition notes :
T wave = electrical recovery
and relaxation of ventricles. A heart attack (myocardial infarction or
MI) can be recognized by an elevation in the S-T segment of the
ECG. Thus, one type of MI is an S-T elevation MI or STEMI.
addition notes :
P wave = spread of excitation wave over the atria just before
contraction;
QRS wave = spread of excitation wave over the
ventricles as the ventricles contract;
T wave = electrical recovery
and relaxation of ventricles.
Atrioventricular node (AV node): This sends the
excitation wave to a bundle of specialized fibers
called the atrioventricular bundle or Bundle of His.
• Bundle of His (pronounced “hiss”): Helps form
conduction myofibers that extend to ventricle walls
and stimulate them to contract, beginning systole. A
short rest period follows.
• The pacemaker begins wave of excitation again.
• ECG or EKG (electrocardiogram): The record used to
detect electrical changes in heart muscle as the heart
beats.
Electrocardiogram. An electrocardiogram (ECG or EKG) records the electrical signal from the heart to check for different heart conditions.
Sinoatrial node (SA node): the pacemaker of the
heart
Pacemaker: origin of electrical impulse causing
walls of the atria to contract and force blood
into the ventricles (ending diastole
Most patients want to get out of the hospital as soon as possible. No one wants to sleep in a loud hospital room with constant interruptions for rounding, vital sign checks, blood work, etc. Hospitals are a place for people when they’re sick, and if you aren’t sick you shouldn’t be in a hospital.
I have noticed a funny thing…often the less ill a patient is, the less they ask about discharge, and the more sick a patient is, the more they focus on going home. A scenario that repeats itself day and day again is as follows (Warning: hyperbole ahead):
Me: “So Mr. Jones, I see here in your chart that you have a history of heart trouble, diabetes, and emphysema. What brought you in today?”
Mr. Jones: “Well I can’t breathe, and I’m passing black tarry stools, and my pacemaker fired three times today during dialysis, and I’m having severe belly pain. Did I mention I can’t breathe?”
Me: “Yes, I can see you’re got a lot going on. Tell me, when did you start having black tarry stools and severe abdominal pain?”
Mr. Jones: “Oh that started a few days ago. When can I go home?”
I guess there is a natural tendency to focus on the light at the end of the tunnel when you are really sick. Maybe fixating on the goal of discharge takes away some of the anxiety of the hospitalization. The thing is, I simply have no idea when a patient with multiple active problems will be able to go home.
No one can really tell when an individual patient will be able to safely leave the hospital after a major illness. I can tell you what the average length of stay is for a certain disease based on past experience, but this number often has little bearing on the individual patient. Everyone is different. The average time in the hospital for an isolated bleeding ulcer requiring blood transfusions and endoscopy may be 2-3 days, however if there are other problems that come up along the way the length of stay may be two weeks. Predicting how long someone has to stay is really just an educated guessing game.
Truth be told, I would rather someone who is sick ask me the impossible question of “when am I going home” than the opposite extreme…
Me: “OK Mrs. Smith, it looks like everything checks out: Your EKG, labs, cardiac enzymes, stress test, and chest X-ray are all normal. The mild vague pain that started two months ago and has since disappeared after antacids is probably just heartburn. I can have you follow up with me in the office next week for any further testing needed.”
Mrs. Smith: “Oh no, I’m not in any rush to leave until I have everything checked out! I want an endoscopy tomorrow. I’m overdue for my mammogram, and I think I just got a letter telling me to schedule my colonoscopy too. My knee has been bothering me for months…do you know any good orthopedists? My daughter is out of town and can’t pick me up from the hospital until at least next Thursday anyway…”
If you enjoyed this article, sign up for our free newsletter and never miss a post!
https://www.sleepfoundation.org/cpap/cpap-vs-bipap UPDATED APRIL 10, 2023
copy from above mentioned website for learning purposes
Written by
Jay Summer, Staff Writer
Medically Reviewed by
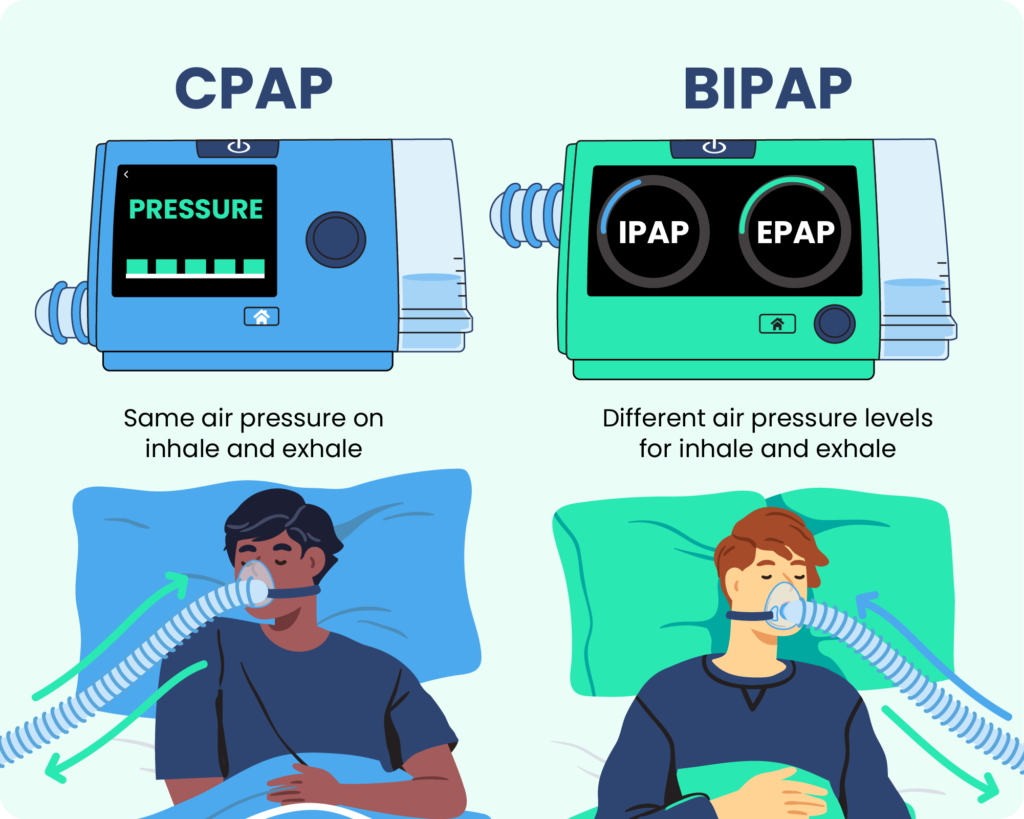
Dr. Abhinav Singh, Sleep PhysicianPositive airway pressure (PAP) is one of the most common treatments for sleep apnea, a breathing disorder that affects approximately 10% to 30% Trusted SourceUpToDateMore than 2 million healthcare providers around the world choose UpToDate to help make appropriate care decisions and drive better health outcomes. UpToDate delivers evidence-based clinical decision support that is clear, actionable, and rich with real-world insights.View Source of the population. The most common PAP treatment is continuous positive airway pressure (CPAP), but bilevel positive airway pressure (BiPAP or BPAP) may be a better option for some people.
While both forms of PAP therapy work in similar ways, their differences mean that each has distinctive benefits and drawbacks to consider. Because of this, the decision to switch PAP treatments should always be made under the advice of your health care team.
CPAP and BiPAP machines are both forms of positive airway pressure therapy Trusted SourceNational Library of Medicine, Biotech InformationThe National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information.View Source , which uses compressed air to open and support the upper airway during sleep. A portable machine generates the pressurized air and directs it to the user’s airway via a hose and mask system. Both systems use similar masks, hoses, and other accessories.
In general, CPAP machines have an adjustable pressure setting that delivers between 4 to 20 cm H2O Trusted SourceUpToDateMore than 2 million healthcare providers around the world choose UpToDate to help make appropriate care decisions and drive better health outcomes. UpToDate delivers evidence-based clinical decision support that is clear, actionable, and rich with real-world insights.View Source (a measure of air pressure that stands for centimeters of water pressure) regardless of whether the user is inhaling or exhaling. The average setting is between 8 to 10 cm H2O Trusted SourceNational Library of Medicine, Biotech InformationThe National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information.View Source . While CPAP machines have only one setting, some models now have a pressure relief option that allows for gentler air pressure on the exhale.
BiPAP machines have two pressure settings — inhalation positive airway pressure (IPAP) and exhalation positive airway pressure (EPAP) — that allow for lower pressure levels during exhalation. Depending on the BiPAP machine’s settings, the switch between IPAP and EPAP may be timed or automatically based on the user’s breathing patterns. BiPAP machines have a typical pressure range of 4 to 30 cm H2O. Both BiPAP and CPAP settings must be determined in an overnight sleep study, or polysomnography.
There are portable CPAP machines designed for travel, while BiPAP machines are designed for at-home use. Because BiPAP machines require additional sensors and settings, they are usually more expensive than an otherwise similar CPAP machine.
Different types of PAP therapy work better for different conditions, though there is some overlap Trusted SourceNational Library of Medicine, Biotech InformationThe National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information.View Source . CPAP therapy is generally recommended for obstructive sleep apnea (OSA), and sleep specialists are unlikely to place someone with OSA on BiPAP unless they cannot tolerate CPAP treatment. While some insurance providers cover both CPAP and BiPAP for OSA, those that do usually require proof that CPAP treatment is inadequate or not tolerated before reimbursing for a BiPAP machine. BiPAP therapy is primarily used to treat central sleep apnea (CSA), as well as heart, lung, and neurological disorders that require structured airway support during sleep.
Both CPAP and BiPAP machines are available with a range of accessories, both integrated and after-market. The most common are data collection features and climate control features like humidifiers and heated tubing.
| CPAP | BiPAP | |
|---|---|---|
| Typical Cost | $500-$1000 | $1,700-$3,000 |
| Pressure Levels | 1 | 2 |
| Typical Pressure Range | 4 to 20 cm H2O | 4 to 30 cm H2O |
| Insurance Coverage | May be covered | May be covered if CPAP therapy fails or is contraindicated |
A continuous positive airway pressure (CPAP) machine directs pressurized air — usually set between 4 and 20 cm H2O — into a user’s airway Trusted SourceNational Heart, Lung, and Blood Institute (NHLBI)The NHLBI is the nation's leader in the prevention and treatment of heart, lung, blood and sleep disorders.View Source while they sleep. This pressure keeps air passages open and ensures the user can breathe properly, allowing them to avoid the pauses in breathing (or apneas) that are the primary symptom of sleep apnea.
CPAP machines continuously pump air at one pressure setting rather than varying in pressure between the inhale and exhale, which can cause some people to feel as though they cannot exhale properly or that they are choking. Most users adjust to CPAP relatively quickly, while others find BiPAP easier to tolerate.
Unlike BiPAP machines, CPAP machines are available in a range of sizes. The most common type is intended to be used at home and is slightly smaller than a shoebox, while travel versions may be small enough to fit in the palm of your hand. Travel models sometimes have backup batteries for use while camping, and FAA-approved models are available for use on planes.
Bilevel positive airway pressure machines have distinct air pressure settings for inhalation (IPAP) and exhalation (EPAP). The EPAP setting is usually significantly lighter than the IPAP setting, allowing users to breathe more naturally and not feel as though they are fighting against the machine when they exhale. Most BiPAP machines have a range of approximately 4 to 30 cm H2O.
BiPAP machines have up to three settings for the switch between IPAP and EPAP.
Additionally, BiPAP machines can be fixed or auto-adjusting.
Although CPAP and BiPAP machines may seem similar, their differences can have a significant impact on your treatment. Because of this, the decision to switch from one to another should always be made with your health care team.
CPAP users usually have an adjustment period before they feel comfortable using their machines. Discomfort can be managed by adjusting settings, experimenting with climate control accessories or different mask types, or using a machine that slightly reduces air pressure on the exhale. BiPAP treatment is available for patients who do not tolerate CPAP therapy, but this switch must be decided on and supervised by a sleep specialist.
Listed news articles do not represent the opinion of Sleep Foundation and are provided for informational purposes only.