https://www.sleepfoundation.org/cpap/cpap-vs-bipap UPDATED APRIL 10, 2023
copy from above mentioned website for learning purposes
Positive airway pressure (PAP) is one of the most common treatments for sleep apnea, a breathing disorder that affects approximately 10% to 30% Trusted SourceUpToDateMore than 2 million healthcare providers around the world choose UpToDate to help make appropriate care decisions and drive better health outcomes. UpToDate delivers evidence-based clinical decision support that is clear, actionable, and rich with real-world insights.View Source of the population. The most common PAP treatment is continuous positive airway pressure (CPAP), but bilevel positive airway pressure (BiPAP or BPAP) may be a better option for some people.
While both forms of PAP therapy work in similar ways, their differences mean that each has distinctive benefits and drawbacks to consider. Because of this, the decision to switch PAP treatments should always be made under the advice of your health care team.
What Is the Difference Between CPAP and BiPAP Machines?
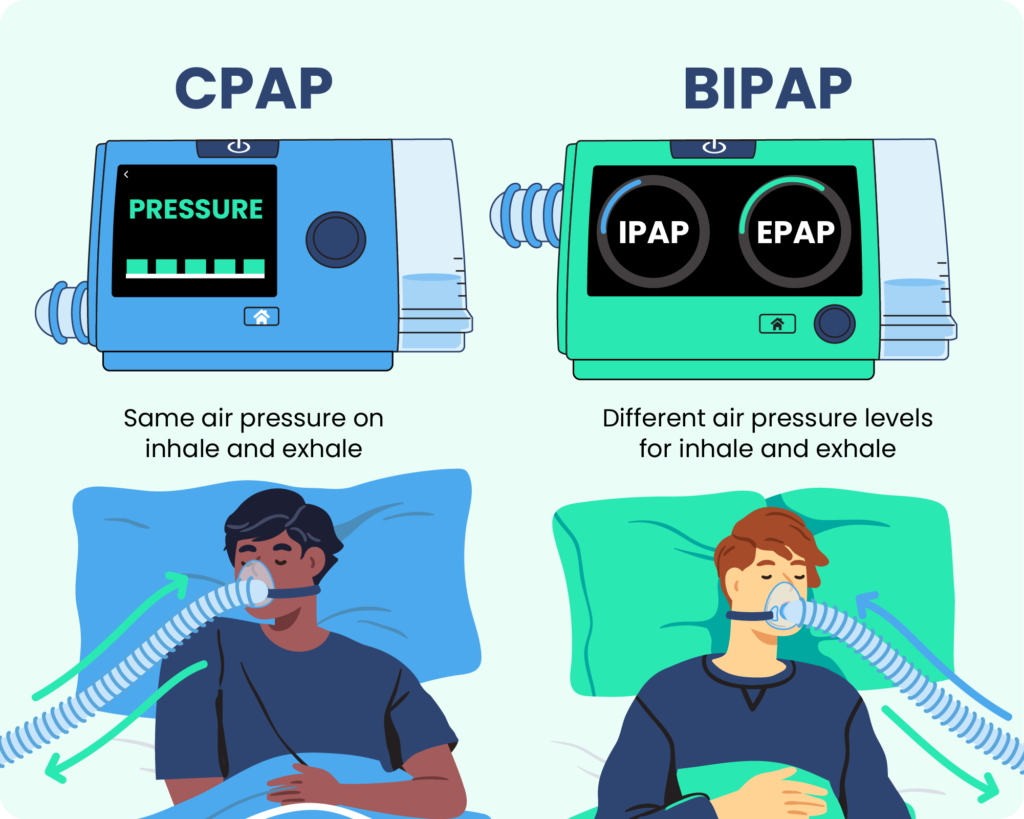
CPAP and BiPAP machines are both forms of positive airway pressure therapy Trusted SourceNational Library of Medicine, Biotech InformationThe National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information.View Source , which uses compressed air to open and support the upper airway during sleep. A portable machine generates the pressurized air and directs it to the user’s airway via a hose and mask system. Both systems use similar masks, hoses, and other accessories.
In general, CPAP machines have an adjustable pressure setting that delivers between 4 to 20 cm H2O Trusted SourceUpToDateMore than 2 million healthcare providers around the world choose UpToDate to help make appropriate care decisions and drive better health outcomes. UpToDate delivers evidence-based clinical decision support that is clear, actionable, and rich with real-world insights.View Source (a measure of air pressure that stands for centimeters of water pressure) regardless of whether the user is inhaling or exhaling. The average setting is between 8 to 10 cm H2O Trusted SourceNational Library of Medicine, Biotech InformationThe National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information.View Source . While CPAP machines have only one setting, some models now have a pressure relief option that allows for gentler air pressure on the exhale.
BiPAP machines have two pressure settings — inhalation positive airway pressure (IPAP) and exhalation positive airway pressure (EPAP) — that allow for lower pressure levels during exhalation. Depending on the BiPAP machine’s settings, the switch between IPAP and EPAP may be timed or automatically based on the user’s breathing patterns. BiPAP machines have a typical pressure range of 4 to 30 cm H2O. Both BiPAP and CPAP settings must be determined in an overnight sleep study, or polysomnography.
There are portable CPAP machines designed for travel, while BiPAP machines are designed for at-home use. Because BiPAP machines require additional sensors and settings, they are usually more expensive than an otherwise similar CPAP machine.
Different types of PAP therapy work better for different conditions, though there is some overlap Trusted SourceNational Library of Medicine, Biotech InformationThe National Center for Biotechnology Information advances science and health by providing access to biomedical and genomic information.View Source . CPAP therapy is generally recommended for obstructive sleep apnea (OSA), and sleep specialists are unlikely to place someone with OSA on BiPAP unless they cannot tolerate CPAP treatment. While some insurance providers cover both CPAP and BiPAP for OSA, those that do usually require proof that CPAP treatment is inadequate or not tolerated before reimbursing for a BiPAP machine. BiPAP therapy is primarily used to treat central sleep apnea (CSA), as well as heart, lung, and neurological disorders that require structured airway support during sleep.
Both CPAP and BiPAP machines are available with a range of accessories, both integrated and after-market. The most common are data collection features and climate control features like humidifiers and heated tubing.
| CPAP | BiPAP | |
|---|---|---|
| Typical Cost | $500-$1000 | $1,700-$3,000 |
| Pressure Levels | 1 | 2 |
| Typical Pressure Range | 4 to 20 cm H2O | 4 to 30 cm H2O |
| Insurance Coverage | May be covered | May be covered if CPAP therapy fails or is contraindicated |
CPAP Basics
A continuous positive airway pressure (CPAP) machine directs pressurized air — usually set between 4 and 20 cm H2O — into a user’s airway Trusted SourceNational Heart, Lung, and Blood Institute (NHLBI)The NHLBI is the nation's leader in the prevention and treatment of heart, lung, blood and sleep disorders.View Source while they sleep. This pressure keeps air passages open and ensures the user can breathe properly, allowing them to avoid the pauses in breathing (or apneas) that are the primary symptom of sleep apnea.
CPAP machines continuously pump air at one pressure setting rather than varying in pressure between the inhale and exhale, which can cause some people to feel as though they cannot exhale properly or that they are choking. Most users adjust to CPAP relatively quickly, while others find BiPAP easier to tolerate.
Unlike BiPAP machines, CPAP machines are available in a range of sizes. The most common type is intended to be used at home and is slightly smaller than a shoebox, while travel versions may be small enough to fit in the palm of your hand. Travel models sometimes have backup batteries for use while camping, and FAA-approved models are available for use on planes.
BiPAP Basics
Bilevel positive airway pressure machines have distinct air pressure settings for inhalation (IPAP) and exhalation (EPAP). The EPAP setting is usually significantly lighter than the IPAP setting, allowing users to breathe more naturally and not feel as though they are fighting against the machine when they exhale. Most BiPAP machines have a range of approximately 4 to 30 cm H2O.
BiPAP machines have up to three settings for the switch between IPAP and EPAP.
- Spontaneous: Spontaneous switching automatically senses the user’s breathing pattern and switches between the two pressure levels when they naturally inhale and exhale. The majority of BiPAP users rely on this setting, and it is standard for BiPAP devices.
- Timed: Timed switching allows users to program how long each IPAP and EPAP phase should last. This ensures users take the correct number of breaths per minute and can function much like a ventilator.
- Spontaneous/timed: This setting is primarily spontaneous, following the user’s natural breathing patterns. On this setting, timed switching turns on when the machine senses that the user has dropped below a set number of breaths per minute.
Additionally, BiPAP machines can be fixed or auto-adjusting.
- Fixed: The IPAP and EPAP settings of a fixed BiPAP machine are pre-set and do not change throughout the night.
- Auto-adjusting: An auto-adjusting BiPAP machine has a range set for both IPAP and EPAP. This allows the machine to adjust automatically throughout the night in response to how the sleeper is breathing.
BiPAP vs CPAP: Which Is Best for You?
Although CPAP and BiPAP machines may seem similar, their differences can have a significant impact on your treatment. Because of this, the decision to switch from one to another should always be made with your health care team.
CPAP users usually have an adjustment period before they feel comfortable using their machines. Discomfort can be managed by adjusting settings, experimenting with climate control accessories or different mask types, or using a machine that slightly reduces air pressure on the exhale. BiPAP treatment is available for patients who do not tolerate CPAP therapy, but this switch must be decided on and supervised by a sleep specialist.
- CPAP Adherence Tied to Fewer Days of Cold Symptoms
March 31, 2023 – A study found that adherence to continuous positive airway pressure (CPAP) therapy may make viral infections less severe in people with obstructive sleep apnea. - People Who Have Morning Chronotype May Show Better CPAP Adherence
March 13, 2023 – Data analysis suggests that people with morning chronotype used their continuous positive airway pressure (CPAP) machine longer each night. - Study Compares How Surgery vs. CPAP Lowers Diabetes Risk in People With Sleep Apnea
- Mindfulness May Be an Additional Way to Increase CPAP Adherence
Listed news articles do not represent the opinion of Sleep Foundation and are provided for informational purposes only.