Test: Alzheimer’s Disease
ALZHEIMER’S DISEASE
Abstract:
No one knows what causes Alzheimer’s disease but certain factors are suspected, such as a person’s genetics, lifestyle, or environment. Health clinicians must be able to distinguish between Alzheimer’s disease, dementia, and the normal aging process. Currently, there is no cure for Alzheimer’s disease but once it is diagnosed, there are treatment options for the patient. A health clinician will need to incorporate medication, behavioral, and communication strategies available for Alzheimer’s patients.
Learning Objectives:
- Identify characteristics of Alzheimer’s disease.
- Knowledge of treatment options for Alzheimer’s patients.
- Understand ways to communicate with individuals diagnosed with Alzheimer’s disease.
Introduction
Alzheimer’s disease is a chronic, incurable, disease that causes devastating damage to the brain and nervous system. The number of people with Alzheimer’s disease is growing. To understand the impact Alzheimer’s disease has on a person, a general understanding of the brain and nervous system function is needed before discussing the causes and risk factors of Alzheimer's disease. Caring for a patient with Alzheimer’s can be one of the biggest challenges a health care professional will face during their career. Because Alzheimer’s disease in the advanced stages causes significant neurological impairments, these patients need considerable assistance to ensure that they are safe and comfortable. Peers and other caregivers will have accumulated experiences and knowledge while working with patients diagnosed with Alzheimer’s disease. Collaboration with other health team members will support the health care professional to care for an Alzheimer’s patient and will help to turn a tremendous challenge into a rewarding experience.
Alzheimer’s Disease: The Scope of The Problem
Alzheimer’s disease is very common. It is the most common cause of dementia. Over 5 million people in the United States suffer from Alzheimer’s disease and by the year 2030, the number of people aged 65 years and older who have Alzheimer’s is expected to grow to almost 8 million. More than 14% of all American adults over the age of 65 have Alzheimer’s disease, and it is considered to be a leading cause of death.
People with Alzheimer’s disease live an average of eight years after the diagnosis is confirmed but some people may survive up to 20 years. Life expectancy and the speed with which the disease progresses depends on the general health of the individual and how early in life they develop Alzheimer’s. A person diagnosed with Alzheimer’s early generally has a poor outcome. Some people have a slow, almost imperceptible progression of the signs and symptoms; other people become debilitated very rapidly and dramatically. Regardless, the growth of the disease weighs on the resources of the patient, the patient’s family, and the health care system.
The Brain, Nervous System, And Alzheimer’s Disease
The brain has many parts, each of which is responsible for particular functions. The following section describes a few key structures and what they do.
Two cerebral hemispheres account for 85 percent of the brain’s weight. The billions of neurons in the two hemispheres are connected by thick bundles of nerve cell fibers called the corpus callosum. Scientists now think that the two hemispheres differ not so much in what they do (the “logical versus artistic” notion), but in how they process information. The left hemisphere appears to focus on details (such as recognizing a particular face in a crowd). The right hemisphere focuses on a broad background (such as understanding the relative position of objects in space). The cerebral hemispheres have an outer layer called the cerebral cortex. This is where the brain processes sensory information received from the outside world, controls voluntary movement, and regulates cognitive functions, such as thinking, learning, speaking, remembering, and making decisions.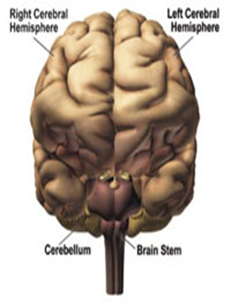
The cerebral hemispheres have four lobes, each of which has different roles. The frontal lobe, which is in the front of the brain, controls “executive function” activities like thinking, organizing, planning, and problem-solving, as well as memory, attention, and movement. The parietal lobe, which sits behind the frontal lobe, deals with the perception and integration of stimuli from the senses. The occipital lobe, which is at the back of the brain, is concerned with vision. The temporal lobe, which runs along the side of the brain under the frontal and parietal lobes, deals with the senses of smell, taste, and sound, and the formation and storage of memories.
The cerebellum sits above the brainstem and beneath the occipital lobe. It takes up a little more than 10 percent of the brain. This part of the brain plays a role in balance and coordination. The cerebellum has two hemispheres, which receive information from the eyes, ears, muscles, and joints about the body’s movements and position. Once the cerebellum processes that information, it sends instructions to the body through the rest of the brain and spinal cord. The cerebellum’s work allows an individual to move smoothly, maintain balance, and turn around without even thinking about it. It also is involved with motor learning and remembering how to do things like drive a car or write one’s name.
The brain stem sits at the base of the brain. It connects the spinal cord with the rest of the brain. Even though it is the smallest of the three main players, its functions are crucial to survival. The brain stem controls the functions that happen automatically to keep people alive, such as the heart rate, blood pressure, and breathing. It also relays information between the brain and the spinal cord, which then sends out messages to the muscles, skin, and other organs. Sleep and dreaming are also controlled by the brain stem.
The brain and the nervous system are considered here separately because the brain is a distinct organ. However, many times the term nervous system is used to refer to the brain, the spinal cord, and the nerves themselves.
Purpose of the Nervous System and Brain
The basic purpose of the nervous system and the brain is to initiate and control involuntary behaviors such as breathing, circulation, digestion, and to initiate and control voluntarybehaviors such as abstract thinking, memory, planning, and solving problems . Everything people do essentially starts and is controlled by the nervous system and the brain. It is helpful to think of the brain as the “command center” and the nervous system as the “wiring,” the carrier that transmits information to and from the brain.
Organization of the Nervous System
The nervous system is composed of the brain, the spinal cord, and nerve fibers. In one sense the brain could be considered the power plant or command center, and the spinal cord and the nerve fibers are the wirings that carry the energy and the messages generated by the brain to the different parts of the body. The nerve fibers and the spinal cord also carry information and messages back to the brain.
How the Nervous System Works
The brain initiates and controls behavior by receiving and sending information. For example, when someone is standing in front of another person, the image of that person is transmitted through the nerve fibers in the person’s eyes to an area of the brain called the cortex that stores information in one’s memory center. When the image reaches the cortex, an individual searches his/her memory, recognizes (or not recognizes) that person, and depending on who they are, triggers a response in a particular way. In this situation, the visual image is carried to the brain by the nerve fibers and the spinal cord to the brain. The brain receives this information and after searching the memory, the brain sends a message to the body through the spinal cord and the nerve fibers.
The information the nervous system sends and receives is carried by tiny electrical impulses and chemicals called neurotransmitters. As mentioned above, the brain is the “command center” and the spinal cord, the nerve cells, and the nerve fibers are the “wiring” that carry information to and from the brain. However, there are short gaps in the connections (the wiring) between the nerve fibers, the nerve cells, the spinal cord, and the brain. These gaps are called synapses and when an electrical impulse reaches a synapse, a neurotransmitter chemical is released and carries the impulse across the synapse to the next part of the nervous system. The drugs that are used to treat patients who have Alzheimer’s disease work by preventing the breakdown of the neurotransmitters that carry the electrical impulses across the synapses.
The nervous system initiates and controls involuntary and voluntary behavior, and different areas of the brain are responsible for specific behaviors. The example given above is a voluntary behavior, but the brain also has many specific areas that control involuntary behavior such as breathing, circulation, and digestion.
How Alzheimer’s Disease Affects The Brain
Alzheimer’s disease causes damage to the cortex, the part of the brain that is responsible for higher mental activities such as memory, problem-solving, language and speech, and abstract thinking. When the brain is examined during an autopsy the most striking finding is the presence of what are called beta-amyloid plaques and neurofibrillary tangles in the cortex. The plaques and tangles are clumps of abnormal tissue that are almost like scar tissue that form inside the cells of the cortex and in the synapses. The plaques and tangles cause irreversible damage to the nerve and brain cells. These plaques and tangles interrupt normal nervous system functioning and the normal functioning of neurotransmitters. Initially, the body tries to repair this damage by an immune system response but eventually, this response stops being helpful and subsequently increases the damage and deterioration. Nerve cells in the brain become dysfunctional and die.
At some point in this progression, the cortex can no longer function and the transmission of information to and from the brain is abnormal and disrupted. People suffering from Alzheimer’s disease, named after the physician who first identified the condition, have difficulty with memory, language, and abstract thinking. They are often confused and disoriented, even in familiar situations and among people they know.
The disease is progressive; once someone develops Alzheimer’s disease, mental functioning begins to deteriorate. In some cases, the progression of damage and the signs of Alzheimer’s disease is slow and subtle, but in others, the damage happens very quickly. When that “tipping point” is reached, a person with Alzheimer’s disease cannot perform the mental activities that allow the person to function and survive. Someone with late-stage Alzheimer’s disease will need to be cared for completely, and this may lead to the patient’s death.
Causes Of Alzheimer’s Disease:
There has been a tremendous amount of research directed towards discovering the causes of Alzheimer’s disease but at this point, no one can say with certainty why it happens or what causes it. Factors such as a traumatic brain injury, obesity, advanced age, high blood pressure, and metabolic problems may contribute to the development of the disease. A small number of Alzheimer’s cases appear to have a genetic component. If a person has a family member who developed Alzheimer’s disease, then that person has a higher risk for developing the disease. This genetic component is found in cases of Alzheimer’s that are called “early-onset” Alzheimer’s. Early-onset is cases in which the signs of the disease develop when a person is age 40s, or slightly younger.
There are defective genes that can cause Alzheimer’s disease but these account for a tiny minority of all cases of the disease. If this gene is defective it may increase the risk for developing the more common type of Alzheimer’s, the late-onset form but not in all cases.
While the cause of Alzheimer’s disease is not known, there appear to be risk factors associated with the disease. There is a higher prevalence of Alzheimer’s disease in women. This may be due to the decline in estrogen production after menopause. Estrogen inhibits some of the pathological processes such as inflammation and oxidative stress that are involved in the development of Alzheimer’s disease. Estrogen also has been shown in animal studies to inhibit and reverse the formation of beta-amyloid plaques and neurofibrillary tangles, the abnormal lesions that are found in the brains of people who have Alzheimer’s disease.
Ethnic background is also a risk factor for the development of Alzheimer’s disease. According to the Alzheimer’s Association, older African Americans are twice as likely as older whites to develop Alzheimer’s disease, and older Hispanics are one and one-half times as likely to develop Alzheimer’s disease than older non-Hispanic whites. These differences do not appear to be caused by genetic factors. More likely, the differences in the incidence of Alzheimer’s between these ethnic groups are caused, in part, by the higher incidence of hypertension and diabetes in the African American and Hispanic populations. Both of these chronic diseases are risk factors for the development of Alzheimer’s disease.
Socio-economic factors and access to health care also make detection and treatment of hypertension and diabetes problematic. This in turn impacts the detection and treatment of Alzheimer’s disease and other dementias related to these conditions.
Myths About Alzheimer’s Disease:
There are many misconceptions and myths about Alzheimer’s disease. These are highlighted here.
Only Older People Develop Alzheimer’s Disease:
Alzheimer’s disease is more common among people aged 65 years and older, but people ages 30s and 40s can develop Alzheimer’s disease.
Alzheimer’s Disease is Very Debilitating but Is Not Fatal:
Many people may not realize that Alzheimer’s disease is one of the leading causes of death.
Exposure to Aluminum Causes Alzheimer’s Disease:
There is no evidence that being exposed to aluminum by using pots and pans made of aluminum or using deodorants that contain aluminum causes Alzheimer’s disease.
Memory Loss of Alzheimer’s Disease is Normal Aging:
There is still no definite evidence that memory loss is inevitable for a person because of aging; moreover, memory loss that is part of Alzheimer’s disease is not normal.
People with Alzheimer’s Disease Don’t Realize Being Forgetful:
Some people in the early stages of Alzheimer’s disease are aware that their mental faculties are getting worse. This knowledge is very frightening and it can worsen the behavior of a person who has Alzheimer’s disease.
Certain Foods, Flu vaccine, and Dental Fillings Cause Alzheimer’s Disease:
There have been rumors and internet myths that certain foods, the flu vaccine, and dental fillings with mercury can cause Alzheimer’s disease but these have all been disproved.
Diagnosis Of Alzheimer’s Disease
Alzheimer’s disease is a diagnosis of exclusion because there are no confirmatory tests for the condition. Other causes of dementia and neurological derangements are ruled out and, if they are not present, a diagnosis of Alzheimer’s disease is made. For example, imaging studies, such as a computed tomography scan (CT) and magnetic resonance imaging (MRI) test and laboratory tests are used to detect a cause for dementia; they do not provide diagnostic evidence of the presence of Alzheimer’s disease.
The exam by the provider should look for multiple deficits in mental and physical functioning such as impaired memory, the inability to recognize familiar objects despite normally functioning senses, an inability to speak or an inability to speak clearly and coherently, an inability to perform simple manual tasks despite normally functioning motor capacity, and an inability to perform higher mental activities. These deficits should be causing serious difficulties in day-to-day living. The deficits should start gradually and get worse over time.
Other causes of the deficit such as a brain tumor, medication side effects, and infection, should have been investigated and ruled out.
An initial screening test that is often used to assess people who may have Alzheimer’s disease is the Mini-Mental Status Exam (MMSE). Examples of questions during the MMSE include:
- Asked the day of the week, and the month.
- Asked to count backward from 100 using intervals of 7.
- Asked to name two familiar objects in the room such as a lamp or a chair when the examiner points to them.
- Asked to say out loud a short list of simple objects, wait a few minutes, then ask the patient to repeat the list.
- Asked to say a short, common phrase, wait a few minutes, then ask the patient to repeat the phrase.
Some individuals might have difficulty performing all of these tasks perfectly if they were tired or anxious, yet may get most of them right. But, for the patient with Alzheimer’s disease, these memory/mental challenges would be far too difficult and confusing. The MMSE is not a test that can be used to definitively make a diagnosis of Alzheimer’s disease. It is a screening tool and, if someone has abnormal results, other tests must be done before it can be determined a person has Alzheimer’s disease.
Alzheimer’s Disease Versus Other Causes of Dementia
There are no specific tests that can confirm the diagnosis of Alzheimer’s disease. However, part of the process in making the diagnosis of Alzheimer’s disease is looking for other causes of the neurological impairment. Alzheimer’s disease is the most common cause of dementia, but there are many others, as well, and these can be confirmed or ruled out by diagnostic testing.
The most common causes of dementia, aside from Alzheimer’s disease are:
- Vascular Dementia
- Parkinson’s Disease
- Chronic Alcohol Use
- Alcohol or Drug Intoxication
Other less common causes of dementia are:
- Huntington’s Chorea
- Multiple Sclerosis
- Hypothyroidism or Hyperthyroidism
- Hypoparathyroidism or Hyperparathyroidism (Cushing’s Disease)
- Head Trauma
- Heavy Metal Poisoning (Lead, Mercury)
- Infection(HIV/Aids or Neurosyphilis)
- Psychiatric Disorders (Depression)
- Cancer
10.Vitamin or Mineral Deficiencies (B1, B3, or B 12, copper)
The presence or absence of these pathologies depends in part on age, access to medical care, socioeconomic factors, geographical locations, and cultural, personal, social, and employment history. A diagnostic workup for dementia to detect one of these might include:
- Blood test for HIV or syphilis.
- Blood tests that measure thyroid function, liver function (in the case of alcohol use disorder), parathyroid function, adrenal gland function.
- Blood and or urine test for the presence of heavy metals.
- Blood test for B vitamin levels or copper.
- Blood and/or urine tests for drug levels, illicit and prescription.
- Blood tests to check for electrolyte disorders, hyperglycemia, or hypoglycemia.
- Lumbar puncture, to test for infectious diseases.
- CT scan or MRI to check for brain lesions, neoplasms, or patterns of injury associated with other neurological causes of dementia.
The provider would also carefully check the patient’s blood pressure. Hypertension is a risk factor for stroke, and a patient with dementia may have suffered an ischemic or embolic stroke. The patient’s gait would be carefully evaluated to check for the presence of Parkinson’s disease. A social history should be obtained to determine if the patient suffered head trauma, if he/she had been exposed at work or anywhere else to toxins or heavy metals, or if the patient has, or had a history of drug or alcohol use disorder and addiction. Finally, a psychiatric evaluation should be performed. This is important because the psychiatric disorder may be mistaken for dementia and also because depression is relatively common in people who have dementia or Alzheimer’s disease. The incidence of depression in people who have Alzheimer’s disease has been estimated to be approximately 30-50%.
Signs And Symptoms Of Alzheimer’s Disease
Alzheimer’s disease is a progressive condition, and patients who have Alzheimer’s typically move through stages of impairment as they get older.
Stage 1
No signs or symptoms of the disease.
Stage 2
Mild signs and symptoms. The patient may occasionally forget a name or a familiar word, but there are no signs or symptoms of Alzheimer’s disease that are obvious.
Stage 3
Mild decline, the patient's family and friends may notice the patient is having difficulties with memory, concentration, or may easily lose an important object such as house keys. May have difficulty functioning socially or at work, may not be able to remember important words, and may not be able to plan or organize very well.
Stage 4
May have many of the same problems listed in the description of Stage 3, but will also begin to experience mood swings and may become inappropriate and withdrawn in social situations. Complex intellectual tasks such as mental arithmetic become very hard to complete, and the patient has great difficulty in planning activities and managing multiple and/or complex tasks. At this stage, a provider should be able to make a diagnosis of Alzheimer’s disease.
Stage 5
Moderately severe decline is typical at Stage 5. The patient’s mental faculties and ability to function worsen. The patient will need help with day-to-day activities because they will not be able to remember a home address, a home telephone number, and may become confused and uncertain about the day or place. However, the patient should not require assistance to eat and use the toilet but caregivers must be constantly present.
The patient must be kept safe while allowing for independence, providing the patient with a sense of security, and coping with inappropriate behavior and emotional lability.
Stage 6
Patients will have severe cognitive decline. Memory and higher mental faculties continue to decline, and the patient may now need help with dressing, eating, and toilet activities. Sleep disorders become common (sleeping during the day and staying awake at night), bladder and bowel incontinence may happen, and the patient may have significant mood swings and personality changes.Many family caregivers cannot cope with the demands of providing the needed level, and around-the-clock care that is needed.
Decisions about placement may need to be made as even with around-the-clock in-home assistance, the demands would be intense. Health care professionals will usually be providing almost constant assistance for personal care and to ensure patient safety. The need to be very flexible and to have good communication abilities and much patience will be important.
Stage 7
Very severe decline and unable to converse, cannot control movement, has no bladder or bowel control, and cannot eat or dress independently. Health care professionals will be providing complete care.
There are many causes of decreased mental function in the elderly and not all people who are over the age of 65, have memory lapses, or confusion have Alzheimer’s. The earliest evidence of Alzheimer’s disease is often a slow, progressive memory loss,but there are other neurological signs and symptoms that can be warning signs of Alzheimer’s disease. Specific examples of the signs and symptoms of Alzheimer’s disease may include:
- Asking for the same information again, and again, forgetting important names, dates, and events.
- Difficulty in balancing a checkbook, following a simple set of instructions such as a recipe, adjusting a thermostat, or using a microwave oven. The person with Alzheimer’s disease may need to re-learn these simple tasks each time.
- Trouble with vision and depth perception while driving or walking.
- Constantly misplacing things.
- Social withdrawal.
- Changes in mood and personality: Confusion, depression, anger, and suspicion that are intense and unusual may be a sign of Alzheimer’s.
One thing that is obvious from the above list is that some of these behaviors, at least initially and when they are mild, can’t be easily measured and seen. They can also be overlooked or misunderstood.
Many people, young and old, have mood swings, forget where they put their glasses, and/or need occasional reminders to help them through the day, but these people do not have Alzheimer’s disease. So what is the difference? Where is the dividing line between occasional memory lapses and behavior changes and Alzheimer’s? The difference is that for people with Alzheimer’s, the behaviors listed above will be persistent, unusual for them, very dramatic, and will get worse over time. Also, these behaviors will seriously interfere with their ability to safely and competently care for themselves.
Alzheimer’s Disease, Dementia, And Normal Aging Process: Definitions And Differences
The terms dementia and Alzheimer’s disease are often used as if they were one and the same. Many people are confused about the definitions and differences between Alzheimer’s disease and dementia, and many people are confused about the differences between the signs and symptoms of the normal aging process and those of Alzheimer’s.
Dementia is simply a word that means a loss of mental ability. It refers to a group of neurological signs and symptoms, and many of these are seen in patients who have Alzheimer’s disease. However, there are many causes of dementia such as Parkinson’s disease, abnormal blood vessels in the brain, infections, traumatic brain injury, stroke, and metabolic problems. Alzheimer’s disease is simply one cause of dementia.
When it comes to the differences between memory loss and changes in mental functioning that happen as people age and the changes that are seen in Alzheimer’s disease, these differences involve mental deficits seen in Alzheimer’s disease that are much more serious and are not part of the aging process. These cannot be easily corrected, seriously interfere with activities of daily living, with someone’s ability to safely provide self-care, and get worse over time. For example, someone who is elderly may forget what day it is or have a hard time learning something new. However, with a little help, that person will quickly remember the day or be able to learn the new task.
Someone who has Alzheimer’s disease may forget what day it is but also the year and the time of day, and no amount of reminding will help. The person with Alzheimer’s disease will not be able to learn something new, regardless of how much help is given.
Treatment Of Alzheimer’s Disease:
Currently, there is no cure for Alzheimer’s disease. The treatment focuses on two areas of care. Firstly, care involves medication treatment that can help the signs and symptoms caused by the disease; and, secondly, a major part of health care for Alzheimer’s patients incorporates behavioral support with a safe and supportive environment.
Medications:
Medications such as donepezil and memantine can help by affecting the levels of neurotransmitters in the brain. Also, antipsychotic drugs, antidepressants, and sedatives can help treat the mood swings and erratic behavior associated with Alzheimer’s disease.
Behavioral Strategies:
Because of the damage to areas of the brain that control language, memory, higher intellectual functions, and to the brain’s neurotransmitter system, the patient who has Alzheimer’s disease has an impaired ability to accurately perceive external stimuli, such as social situations and conversations. The neurological system damage also impairs the patient’s ability to process new information and to express thoughts and feelings. These limitations make it difficult and at times confusing, and frustrating to interact, attain goals, solve problems, and cope with stress. As a result, behavioral problems that are frightening and/or harmful to the patient and the caregiver may occur. Some of these behaviors may include aggression, anxiety, agitation, confusion, repetition, suspicion, and wandering.
What is difficult for the caregiver of a patient with Alzheimer’s disease is that these behaviors are often extreme, unpredictable, and happen without warning. From the standpoint of a family member or a caretaker, there is no apparent cause for the patient to act out. However, when carefully considering what the patient is doing and what happened immediately before the behavior started, it can often be determined.
The key is to remember that the patient with Alzheimer’s disease has a diminished mental capacity and many times the patient will act out because he/she cannot cope with stress. Stress is the basic cause for many of the disturbing behaviors that can be seen in patients with Alzheimer’s disease. Stress is a normal part of life, but because these patients have diminished mental capacities, even simple, non-threatening situations can be beyond their coping abilities. Situations that most people could easily understand and problems that most would easily solve are overwhelming for the patient with Alzheimer’s disease.
The patient with Alzheimer’s disease has a limited ability to cope with stress. Specifically, these patients can be disturbed by the following conditions.
- Physical Discomfort
The Alzheimer’s patient may be uncomfortable or in pain but will be unable to identify this fact, express themselves, or help
themselves.
- Over-stimulation
Loud noises or an exceptionally active environment can confuse and upset the patient.
- Unfamiliar Surroundings
If the surroundings are unfamiliar, this too can cause fear, anxiety, and confusion.
- Complicated Tasks
A patient with Alzheimer’s is often unable to perform complicated tasks. They can be easily frustrated and act out.
- Complex Interpersonal Interactions
A patient with Alzheimer’s disease can get overwhelmed by long conversations and complex social situations.
The reactions of an Alzheimer’s patient to stress, such as aggression, anxiety, agitation, confusion, wandering, repetition, and suspicion, are understandable when considering that the average person also encounters situations that are too stressful to cope normally. When in a new, unfamiliar situation, it is normal for most people to feel anxious and confused. And when frightened, most people may even feel and act a little aggressively. However, most individuals can assess a new situation and plan an appropriate behavior that will help them cope. But, the patient with Alzheimer’s disease simply has a much lower level of tolerance for these stressors and a diminished ability to adjust to them. As a result, they act out in ways that seem inappropriate.
With patience and planning, health care professionals can successfully manage situations in which the Alzheimer’s patient is agitated, confused, or suspicious. Caregivers can also adjust the environment so that these patients do not become emotionally upset or act out physically. The Alzheimer’s Association (www.alz.org) recommends the following step-by-step approach.
Identify and Examine the Behavior:
First, health care professionals should identify the patient’s behavior and determine whether or not it may be harmful to the patient or others. If it may be harmful or puts someone at risk, decisive steps should be taken to stop the behavior. The health care professional should avoid reacting to the patient, and create a plan of action.
Physical restraints should be used only as a last resort and only if a supervisor or a physician has ordered their use. There are situations in which the use of physical restraint is necessary to stop this behavior, but using physical restraint can be very risky for the patient and the staff. All employers should have clear-cut policies and procedures that explain when and how to use physical restraint. They should be read and understood before ever attempting to use them.
Identify the Cause:
Attempt to identify the “trigger” that might have caused the behavior. Remember, for the patient with Alzheimer’s disease, small changes or disruptions in the environment or the daily routine can be disorienting and upsetting. Identifying the trigger can help in removing or changing the stimulus for the behavior and can also help in managing future stress.
Identify Solutions:
It can be challenging to identify solutions because it is difficult to put oneself in the place of a patient with Alzheimer’s disease. But health care professionals should be flexible, and be able to identify new ways to solve the problem and defuse the situation.
In terms of specific behaviors, the following are therapeutic approaches that can help the patient who has Alzheimer’s disease cope with stressful situations.
- Anxiety:
- The source of the patient’s anxiety should be identified and the stimulus removed. The patient should be gently and consistently reassured that they are in familiar surroundings and with familiar people.
- Aggression:
- The patient should be protected against self-harm and others protected without being confronted or engaged in an argument. Health care professionals should avoid being aggressive and should gently remove the patient from the situation. Distract them with something familiar and comforting if possible.
- Agitation:
- The cause of the patient’s behavior should be identified. Changing the environment or removing the stimulus while gently and consistently reassuring the patient that they are in familiar surroundings and with familiar people can help to de-escalate the patient from being agitated.
- Confusion:
- When explaining something to a patient with Alzheimer’s disease who is confused, explanations should be simple and short. Stay calm, attempt to find familiar cues, will orient the patient to time, place, and people, and help to ameliorate the patient’s confusion.
- Repetition:
- It is important to understand that the patient with Alzheimer’s disease is repeating behavior or a conversation to try to comfort themselves. The patient should be allowed to express themselves while the source of the patient’s anxiety or fear is explored.
- Suspicion:
- Suspicious behavior is almost always triggered by change. It can also be triggered by not remembering who someone is, even if it is a relative or a long-term caregiver. Family and caregivers should avoid being offended, and try to use logic, or common sense to “make the patient understand.” Rather, they should simply, gently, and consistently try to reassure the patient that they are in a familiar environment with people they know and that they are safe.
- Wandering:
- Wandering is a very common behavior in patients with Alzheimer’s disease, and can be very dangerous. Wandering can be reduced by encouraging physical activity and providing the patient with appropriate stimulation. The patient should be protected by encouraging them to wear a Medic Alert bracelet.
Communication Strategies:
The Alzheimer’s Association recommends some specific approaches to the difficult behaviors of those with Alzheimer’s disease, such as suspicion and aggression, which are commonly seen. In a general sense, it is always best to remain flexible, patient, and calm with Alzheimer’s patients.
Threats should never be used. For example, “If you don’t stop behaving this way, I will have to take you back to your room.” Such statements generally will not work for several reasons. Firstly, the patient with Alzheimer’s disease may not understand even if it is pointed out what he/she is doing or why it is wrong. Secondly, a threat requires a person to appreciate a future event, a consequence, that someone who has Alzheimer’s disease is unable to do, or has a limited ability to do. Finally, the patient’s behavior is a reaction to stress.
Arguing with the patient also generally isn’t useful, because they simply cannot understand logic or common sense when upset. People who do not have Alzheimer’s disease often cannot “listen to reason” when they are confused and upset, so it is pointless to expect someone who has Alzheimer’s disease to respond to logic. Being gentle and providing instructions that the person with Alzheimer’s can find simple to understand is very helpful. Gently repeating instructions as often as needed and being willing to change what is said and how it is said so the patient can understand is a very helpful approach.
Behavior should never be taken personally. The patient with Alzheimer’s disease who is acting aggressively or anxiously in a way that seems inappropriate is simply responding as best they can to what they find confusing and anxiety-provoking. Health care professionals and families should look for the source of behavioral dysregulation; it may be a lack of sleep, a medication side effect, or simply a change in surroundings.
What about the patient who has Alzheimer’s disease who is non-communicative or non-responsive? In these situations, the best approach is to take time and to be predictable. As with any patient who has Alzheimer’s disease, the health care professional should make sure the uncommunicative/unresponsive patient is physically comfortable, not over-stimulated, not confronted with unfamiliar surroundings or new situations, and is not asked to do anything complex.
Anything done with these patients or said to them must be done slowly and carefully, and it is best to establish routines. Organizing the day and the activities of daily living so that everything is done slowly and predictably. Always allowing for extra time.
Summary
There are no specific tests that can confirm the diagnosis of Alzheimer’s disease. Alzheimer's disease is the most common cause of dementia, but other sources can be confirmed or ruled out by diagnostic testing.
Patients diagnosed with Alzheimer’s disease react to stress with primary symptoms of aggression, anxiety, agitation, confusion, wandering, repetition, and suspicion. They experience stress the same as most people when exposed to unpredictable or new situations, however, the person with Alzheimer’s is unable to cope normally with stressful encounters and can become confused and escalated. The patient with Alzheimer’s disease will also have difficulty performing on the MMSE, which is a screening tool for abnormal responses related to orientation, memory, and focus/concentration. Alzheimer’s disease is a diagnosis of exclusion. Other causes of dementia and neurological derangements are ruled out using imaging studies and laboratory tests. If no other source is identified, a diagnosis of Alzheimer’s disease is made.
The Alzheimer’s Association recommends some specific approaches to the difficult behaviors of those with Alzheimer’s disease, such as suspicion and aggression. Health care professionals need to remain flexible, patient, and calm when working with Alzheimer’s patients. This will improve communication with the patient and by promoting a predictable routine the patient should feel safe and supported.